Rhabdomyolysis – Symptoms, Treatment, Causes, Diagnosis, Pathophysiology
What is Rhabdomyolysis?
Rhabdomyolysis is an illness that is a result of speedy break down of the skeletal muscle that releases the myoglobin into blood. This myoglobin is a protein that carries oxygen and can be found generally in the muscle. It is not normally released in the bloodstream because the myoglobin will be filtered by the kidneys for excretion. The kidneys don’t usually filter them because it has big molecular component and it can cause toxicity to the renal tubular epithelium of the kidneys. The myoglobin is not totally toxic in nature but it has a ferrihemate part that releases free hydroxyl radicals which are highly nephrotoxic thus may lead to acute renal failure.
Presence of myoglobin in the blood is abnormal but a relevant mark that detects a muscle injury especially if it involves the heart’s muscle.
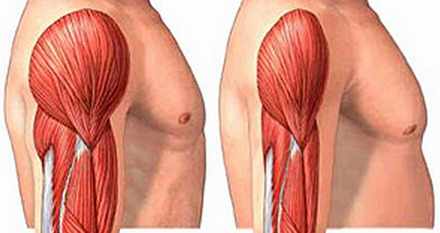
Picture of rhabdomyolysis showing muscle mass loss (right)
Pathophysiology
When muscles cells are damage directly by trauma or by cell metabolism, the fluids will shift from extracellular compartment (bloodstream) into the cells which cause it to swell and put pressure against the nerves and the surrounding tissues. This pressure occludes the blood supply to the muscle and may damage the muscle cells.
The shifting of fluid to the cells causes less circulating fluid in the bloodstream, low blood pressure, and possibly, shock. There will be less blood flow to the kidneys to supply the nutrients and the oxygen it needed to function. It creates further harm to the kidneys resulting to renal failure when Calcium binds to the damaged muscles cells. There begins series of persistent muscle contractions as well as depletion of Adenosine Triphosphate that give rise to the fragmentation of the cell and release of the proteins to the bloodstream. The proteins such as the myoglobin may accumulate in the tubules of the kidney and is highly nephrotoxic. The myoglobin attaches itself to the Tamm-Horsfal protein found in the kidneys’ nephrons to form solid aggregates that occludes the blood flow. The condition worsens when there’s presence of high levels of uric acids that further damage the kidney cells.
Causes &Risk factors
The main cause of the Rhabdomyolysis is the muscle injury like:
Direct muscle injury
- Severe extensive burns
- Physical torture and abuse
- Car accidents
- Prolonged surgery
- Crush Syndrome
- Electrocution
Severe muscle contractions due to
- Intense physical work-out
- Prolonged involuntary muscle contractions during seizures and epileptic episodes
- Delirium Tremens in persons who suffer alcohol withdrawal
- Tetanus – muscle spasms such as Risus Sardonicus (facial spasms), lockjaw, and Opisthotonos.
Metabolism
During the shortage of the Adenosine Triphosphate in generating energy in muscle, the body compensates by breaking down the fat and protein reserves in the muscle to be used as ATP.
Decrease in the level of electrolytes such as phosphates, potassium, calcium that are essential for the production of ATP.
- Hyperthermia and heat stroke
- Hypothermia
- Prolonged immobilization – patients who have been lying on bed for a long time and the hard surface of the bed may put weight against the muscles that can be enough to bring injury to the muscles.
- Drug abuse such as cocaine, amphetamines, and heroine
- Medications such as statins (simvastatin, lovastatin, atorvastatin), anesthesia, psychiatric medications (antidepressants, hypnotics, antilipemic agents)
- Bacterial and Viral Infections by Epstein-Barr Virus, Herpes, HIV, Influenza A virus
- Autoimmune diseases such as polymyositis, sickle-cell disease and dermatomyositis
Symptoms & Signs
Mild symptoms
- Muscle tenderness, pain, swelling
- Muscle weakness
- Dark cola-colored urine
Severe symptoms
When there is acute renal failure the severe symptoms starts, which are like
- Swelling of the upper and lower extremities
- Compartment Syndrome – the fluids from the bloodstream shifts to surrounding tissues like the lungs (causes shortness of breath), muscles that may lead to low blood pressure and shock.
- Electrolyte Imbalance
- Decreased and/or absent urine output
- Lethargy
- Disorientation and confusion
- Irregular heart rate and rhythm
- Comatose
Diagnosis
In detecting the presence of Rhabdomyolysis, it usually suspected to persons who had trauma or accident and the diagnosis of the Rhabdomyolysis begins by physical examination and the history of past and recent events done by the health care practitioner. It is to assess the person’s history if there are obvious trauma present, the severity of the damage, medication use, or if there is an underlying disease that causes it. This relevant information will help to focus what will be the management for the illness.
In addition to that, there are various diagnostic examinations that are indicated to be performed for persons who are suspected with Rhabdomyolysis:
- Blood tests
such as the complete blood count, prothrombin time (PT), partial thromboplastin time (PTT), and electrolytes.
- An electrolyte such as Potassium tends – to increase in the severe form of Rhabdomyolysis. There is also a decrease in Calcium levels because calcium binds to the damage cells.
- Electrocardiography (ECG) reflects the elevated Potassium level by the presence of T wave and broad QRS Complex.
- Kidney function tests such as the Blood Urea Nitrogen (BUN) and Creatinine are done to measure the kidneys’ ability to filter the blood and excrete the body waste via the urine.
- Urinalysis, in the other hand, is also helpful to confirm if myoglobin is present in the urine which is an abnormal result.
- Creatinine Kinase (CK) test is the most reliable diagnostic examination in confirming the presence of Rhabdomyolysis. The Creatinine Kinase is an enzyme released by the muscle if there is an injury done in the muscles. It is usually high and continues to rise during the first twelve (12) hours after the muscle injury and then falls gradually after 1 to 3 days. It is a sensitive marker to confirm the Rhabdomyolysis because once the Creatinine Kinase level failed to decrease 3 days after the injury, it is indicated that the Rhabdomyolysis is present. Since it is present in the cardiac muscle and the brain, the laboratory exam can distinguish which muscle cell is affected by performing CK-MM for skeletal muscles and CK-MB for the cardiac muscle.
- Imaging Studies such as CT Scans and X-Ray are done to visualize the suspected fractures, possible presence of cerebral edema, the extension of brain trauma, and possible seizure activities.
Treatment
Medical Care
Medical Care for the person with Rhabdomyolysis depends on the severity of the illness:
- If the patient has the mild form of Rhabdomyolysis, home treatment takes place by doing rehydration. Drinking a lot of fluids and rest will work.
- On the other hand, home therapy is not applicable for those who have the severe form of the Rhabdomyolysis for it requires intensive monitoring of the electrolyte levels, acid-base balance, urine pH levels, ECG tracings, and the metabolic activities.
- Intravenous infusion is done to avoid the symptoms of shock caused by the Compartment Syndrome. Infusion of large amount of saline increases the flow of fluid to the kidneys, dilute the toxins such as the myoglobin, and correct the levels of electrolytes and the acid-base balance. Mannitol and Furosemide is used to enhance the osmosis and urine production to reduce the kidney damage.
- It is important to monitor the urine output of the patient hourly by inserting an indwelling foley catheter.
- Correction of the levels of Potassium and Calcium to remove the risk of developing fatal dysrhythmmia, ventricular tachycardia, and/or ventricular fibrillation. It also removes the risk of alkalinization of urine that possibly causes acute tubular necrosis (ATN).
- Transfusion of blood products such as the fresh frozen plasma (FFP), platelets, fresh whole blood (FWB) if the complication of Disseminated Intravascular Coagulation is present.
- To preserve the kidney function is one of the focuses of the treatment and dialysis may be required for the patient with renal failure, consistent hyperkalemia and electrolyte imbalance, metabolic acidosis, congestive heart failure, and pulmonary edema to filter the unnecessary body wastes such as the myoglobin that the failed kidneys can’t filter.
- The person should avoid medications that are nephrotoxic that will aggravate the renal failure.
Surgical Care
- This is necessary depends on the severity of the Compartment Syndrome and pressure to perform the fasciotomy. Normally, high pressure of >30 mm Hg is required to perform the fasciotomy.
- Orthopedic and surgical treatment are done to correct the fractures caused by the trauma.
Prognosis
The patient’s chance to recover from Rhabdomyolysis is favorable as long as it is detected on the early stage and given the proper treatment to avoid the further damage to the kidney. Mortality rate for Rhabdomyolysis is approximately 5% but it still depends on the health status of the patient, the severity of the muscle trauma, the kidney function, and presence of complication. It increases to 20% if kidney failure is present.
Complications
There are three complications the Rhabdomyolysis causes:
1. Compartment Syndrome
It is a condition that happens during an injury that causes shifting of the fluids to third spaces and the muscles which causes swelling and increase in pressure within the surrounding tissues where leads to occlusion of the blood supply to the muscles and compression of the nerves, thus loss of blood supply and possible death of the muscle and the nerve.
2. Disseminated Intravascular Coagulation
A pathological condition where bleeding occurs because of blood coagulation impairment. It is detected by diagnostic examinations such as the PT and PTT.
3. Kidney Failure
The myoglobin released by the muscle to the bloodstream will be filtered by the kidneys and has ferrihemate part that is highly nephrotoxic that may cause renal failure. In addition to that, the shifting of fluid from the bloodstream to the intracellular compartment may cause decreased blood flow to the kidneys. It deprives it of blood, oxygen, and nutrients that are essential for kidney function.
Prevention
Rhabdomyolysis is prevented to be developed if the proper management is implemented after the injury. It involves the
- adequate hydration
- exercising the range of motion to aid the muscle trauma and a lot time for resting