Gallbladder Pain – Location, Causes and Treatment
What is Gallbladder Pain?
Pain is a displeasing sensation that can vary from a discomfort to a point of distress. It may be caused by external or internal stimuli which disrupt the normal functioning of a certain body part or the whole body.
Gallbladder pain is elicited either by the formation or blockage of gallstones in the biliary tracts called cholelithiasis or by an inflammation; a condition called cholecystitis.
Biliary colic is a specific term especially used if the pain is situated at the right upper abdomen, where the gallbladder is located. Although colicky pain literally means it comes and go. In biliary colic it does not come and go, it is constant but may fluctuate from time to time. This should be noted so as to prevent confusion.
Gallbladder location
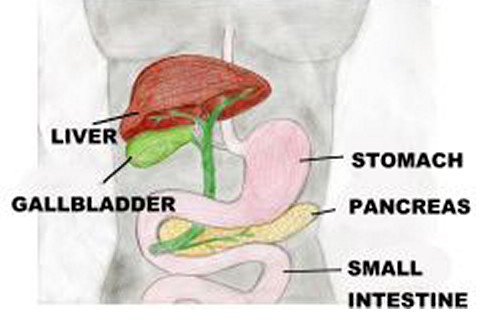
The gallbladder is a small, pear-shaped saclike organ situated in a depression under the right lobe of the liver. The gallbladder consists of an outer serous peritoneal coat, a middle muscular coat, and an inner mucous membrane that is continuous with the linings of the ducts.
Its primary role is to store bile produced by the liver until the next food intake.
Causes and Risk factors
Cholelithiasis is the existence of calculi in the gallbladder. Usually, this is form by solid constituents. Two major types of gallstones are pigment stones and cholesterol stones. In pigment stones, they are formed by unconjugated pigments in the bile precipitate to form stones while in cholesterol stones, although cholesterol is a normal constituent of the bile, its insolubility to water can cause stone precipitation.
Cholecystitis has 2 subcategories that contribute to its presence. Calculous type is with the presence of gallstones. They block the normal flow of the bile thus causing an inflammation which leads to sever pain. Acalculous type is the absence of gallstones but the pain experienced is the same with the calculous type. This type may be caused by severe trauma, burns or after a major surgical procedure.
The aforementioned conditions play vital roles in the production of pain or biliary colic.
There are certain numbers of factors that can cause gallbladder pain. And there are some people who are more prone to this condition, such as:
- Overweight
- Thyroid illness
- Allergies especially in food
- Usage of birth control pills or intake of hormone supplements
- Age above 40
- Women who already gave birth
- High fat, low fiber diet
- Diabetes
- Crash diet
Signs and Symptoms
Although the patient will experience an excruciating pain in the right upper abdomen that radiates to the back and right shoulder, there are other symptoms that accompany pain like:
- Nausea with or without vomiting
- Excessive sweating
- Generalized body weakness
- Light-headedness
- Shortness of breath
- Abdominal bloating/ belching
- Inconsistent bowel movement
Diagnosis
Abdominal X-ray
When a gallbladder blockage is suspected, an abdominal x-ray may be obtained to exclude other causes of the symptom. However, this diagnostic procedure is not just specific to a disease it is very convenient and can immediately give out an idea if the gallbladder is blocked.
If the result is inconclusive, CT scan or MRI should be used; far advanced methods than the traditional one which utilize highly developed equipments.
CT scan stands for computerized tomography scan and this is a method of X-ray slice that takes ‘slice’ of the body cross section or longitudinal section.
MRI, on the other hand, is Magnetic Resonance Imaging does not have X-ray but is very useful in examining the bile ducts.
There are various ways to detect gallbladder disease which is not included in this article. In gallbladder pain, the determination of the cause is the priority and rule out inappropriate diagnoses.
Treatment
When the cause of gallbladder pain has been detected appropriate treatment should be rendered. If the pain is caused by gallstones, there is the surgical and non surgical removal.
Non Surgical
- Dissolving gallstones; infusion of a solvent (mono-octanoin or methyl tertiary butyl ether) into the gallbladder. This method is not widely used.
- Lithotripsy, this is a non-invasive procedure which uses repeated shock waves directed at the gallstones in the gallbladder or common bile duct to fragment the stones.
Use of medication is also popular in the removal of stones. Ursodeoxycholic acid (UCDA) and chenodeoxycholic acid (chenodoil or CDCA) have been used to dissolve small gallstones composed primarily of cholesterol. Treatment with UCDA can reduce the size of existing stones, dissolve small stones, and prevent new stones from forming.
Nutritional and supportive therapy
Almost all patients who had gallbladder pain caused by stones achieve remission after rest, IV fluids, analgesia, and antibiotic agents.
Diet required is usually limited to low fat liquids. These can include powdered supplements high in protein and carbohydrates stirred into milk. Foods that are well tolerated by the patient are encouraged like rice, lean meats, non gas-forming vegetables and fruits, coffee and tea. The patient should avoid eggs, cream, fatty foods, cheese, rich dressings, gas forming vegetables, and alcohol.
Surgical
Cholecystectomy
The gallbladder is removed through an abdominal incision, usually right subcostal after the cystic duct and the artery are ligated. The procedure is performed after an acute or chronic pain episode.
Laparoscopic Cholecystectomy
This procedure replaced the traditional cholecystectomy that requires an incision to remove the gallbladder. It has become the new standard for therapy for symptomatic gallstones. Advantages of laparoscopic procedure are that the patient does not experience the paralytic ileus that occurs with traditional open surgery and has less post operative abdominal pain. The patient is usually discharge same day or within 2 days and can resume full activity after the surgery.
Conversion to the traditional open abdominal surgery may be necessary if problems are encountered with this advanced procedure.
Although the patient is discharged immediately after surgery, he/she may experience drowsiness, so the patient needs assistance in the first 24-48 hours.
 Image source – wikipedia.org
Image source – wikipedia.org