Erythema Multiforme
What is Erythema Multiforme?
A skin condition proposed to be a result of hypersensitivity reaction from drugs or infectious agents. erythema multiforme is characterized by red to pinkish papules, macules and the hallmark “target lesions” that are distributed throughout the limbs and sometimes the mucus membranes.

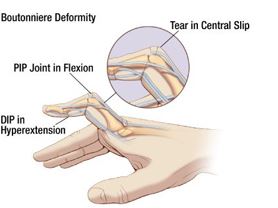
Image 1 – Erythema multoforme on body
When Does Erythema Multiforme Happen?
The red (erythema) rashes usually emerge after exposure to a drug or an infectious agent, for this erythema multiforme is considered as an allergic reaction to a particular agent.
Erythema Multiforme Presentation
The emergence of the rash would vary from a self-limited rash to a life-threatening, severe one. Rash can present itself as small pink macules or papules, and as the condition progresses, the rash becomes large and widely distributed. Erythema multiforme rashes are usually located on the extremities, and rarely may involve the mucous membranes.
The hallmark sign of multiform erythema rash is its target like appearance. Here the lesions appear pale on the center, and pink-red around the circumference. It can also be itchy (as in mild cases) and can cause abrasions and scratches in severe cases when the itching escalates.
Erythema Multiforme Symptoms and Signs
- Itching or burning sensation on the site of the rash
- Numerous red-pink maculo-papular rash that begins on the extremities then may proceed to the torso
- Sharply demarcated pink to red rash
- Presence of a target like lesion (also called “iris” lesion)
- Presence of plaques
- Plaques or papules that have a darker, brown, purpuric, center (happens at the late stages of the condition)
- Presence of blisters and crusting on the center of the lesion may also be noted.
- Presence of mucosal lesions especially in the mouth
Other Signs and Symptoms may include:
- Fever
- Muscle pain
- Body malaise or weakness
- Cough or sore throat
- Joint pain
Erythema Multiforme Causes
Since this condition is a hypersensitivity reaction, the following agents are seen to cause erythema multiforme:
- Herpes Simplex Virus (HSV) – This is the most common agent seen to cause erythema multiforme, almost 50% of the cases are attributed to infection of the herpes simplex virus. HSV has the capability to express its DNA on skin cells, particularly keratinocytes. When their genes are expressed in these cells, our body’s defense system forms killer cells to destroy the viral genes within the skin cells since it is a foreign body. The destruction of the HSV gene also causes the keratinocytes to be destroyed, and this process sparks the inflammatory reaction we seen in erythema multiforme.
- Mycoplasma pneumoniae – Another infectious agent seen to cause erythema multiforme is Mycoplasma pneumoniae. This is an agent that causes fungal infections especially in children. The toxins released by this fungal agent may be the cause of rash and lesion formation seen in erythema multiforme.
- Medications such as:
- Barbiturates
- Penicillins
- Sulfa drugs or sulfonamides
- NSAIDs or non-steroidal anti-inflammatories
- Hydantoins
- Phenothiazines
- Vaccines for:
- Hep B
- Small Pox
- Hepatitis C
- Varicella Zoster
- Cytomegalovirus
- Human immunodeficiency virus
- Dipthteria-tetanus
- New medications are also related to erythema multiforme formation:
- Rofecoxib (Vioxx)
- Candesartan cilextil (Atacand)
- Ciprofloxacin (Cipro)
- Metformin (Glucophage)
- Bupropion (Wellbutrin)
- Adalimurab (Humira)
Erythema Multiforme Diagnosis
Clinical Assessment
Simple assessment of the patient for the presence of target lesions is enough to diagnose erythema multiforme. Further strengthening the diagnosis is the presence of an HSV infection
Skin Biopsy
This is done when the clinical manifestations are not clear. For patients with recurring erythema multiforme or for those with no history of HSV infection, skin biopsy may be done.
Laboratory Tests
Laboratory tests such as Immunoglobulin M and G, HSV-1 and 2 may also be done if the clinical presentation is unclear.
Erythema Multiforme Differential Diagnosis
Many conditions also resemble the clinical presentation of erythema multiforme. Differential diagnosis is important to rule out other forms of condition from erythema multiforme. Differential diagnoses for this condition include the following:
- Urticarial and urticarial vacuities
- Vasculitis
- Viral exanthems such as measles
- Polymorphic light eruption
- Lupus erythematosus
- Pityriasis rosea
- Steven-Johnson’s syndrome
- Drug eruption
- Toxic Epidermal necrolysis
It is important for the physician to take note of the distinguishing characteristics of erythema multiforme. This condition is usually fixed and present for at least one week, and lesions have the characteristic “iris” appearance or the so called “target-like” lesions. Other lesions only emerge for less than 24 hours (urticaria), and do not resemble the target appearance of erythema multiforme.
Erythema Multiforme Treatment
Oral Antihistamines and Steroids
This relieves the symptoms of inflammation such as redness and itchiness. These medications work by suppressing the release of chemicals that cause the inflammatory reaction of redness and itching.
Side effects of antihistamines and steroids
Antihistamines can cause dizziness, and so it must not be taken with alcohol or sleeping pills. Short term steroid use can cause sudden weight gain, facial flushing and increase in appetite. If steroids are used for a long period of time, gastric acidity and immunosuppression are the common side effects.
Oral Acyclovir
Oral acyclovir is given to patients with ongoing HSV infection. Acyclovir is an antiviral drug that destroys the virus and prevents it from replicating. Acyclovir lessens the duration of the eruptions and so is the number of lesions
Side effects of Oral Acyclovir are he following:
- Nausea
- Abdominal pain
- Vomiting
- Dizziness
- Confusion
Prednisone
Prednisone 40-80 mg/day is given for patients with multiple lesions. Its dosage lessened gradually as the lesions subside. Prednisone has an anti-inflammatory effect, suppressing the immune response that causes the inflammation we see in erythema multiforme
Side effects of prednisone
- Water retention
- Insomnia
- Abdominal pain
- Osteoporosis
- Facial swelling
Valacyclovir and Famciclovir
This is given for patients with recurring condition and does not respond to Acyclovir treatment. A dose of Valcyclovir 500-1000 mg and Famciclovir 120-250 mg per day can be given. These are antivirals which halt the viruses’’ capability to strike damage to the cells.
Dapsone treatment
This is given for those with recurrent erythema multiforme who are not responsive to antiviral therapy. Dapsone 100-150 mg per day is given and is seen to partially and completely relieve erythema multiforme. Dapsone has anti-inflammatory and immunosuppressing action, this mechanism helps in suppressing erythema multiforme.
Side effects of Dapsone
- Headache
- Possible hemolysis (related to doses given)
- Nausea
- Peripheral neuritis
Azathioprine or Immuran
This is given if other treatments were not effective; Azathioprine has immunosuppressing effects, modulating the overactive immune response we see in erythema multiforme. This is a potent drug which suppresses the production of chemicals that spark the immune response.
Side effects of Azathioprine or Immuran
- Susceptibility to other infections (because of bone marrow suppression)
- Fatigue
- Hair loss
- Nausea
- Can be a carcinogen if used as a long term treatment
Erythema Multiforme in Children
In children, erythema multiforme is commonly caused by an infection rather than exposure to medications. Primarily causing erythema multiforme in children is the Herpes simplex virus and Mycoplasma pneumoniae. Since this is an infection, erythema multiforme in children is most often coupled with other symptoms such as fever, body weakness, sore throat, muscle pain and joint pain.
Is Erythema Multiforme Contagious?
No, erythema multiforme itself is not a contagious disease. This is a condition that is caused by an allergic reaction to medications or an inflammatory reaction to viruses and fungi. Erythema multiforme is not indicative of a contagious disease and must not be mistaken as a sign of measles and other viral exanthems.
Erythema Multiforme Terminology
Erythema Multiforme Major
This is a severe life-threatening form of erythema multiforme; this type can be related to Steven-Johnson’s syndrome. A condition characterized by severe allergic reactions. Severe allergic reactions can cause anaphylactic shock, the event where a person’s airway is blocked and the blood pressure drops due to severe allergic reaction.
Erythema Multiform Minor
This is the less severe and most common form of erythema multiform. This is highly associated with a Herpes simplex infection. This form is only limited to cutaneous lesions, and is not systemic as compared to erythema multiform major.
Bullous Erythema Multiforme
This type of erythema multiform is characterized by bullous lesion formation. A bullous lesion is a type of a large lesion that contains fluid. In bullous erythema multiform, the rash may initially appear small and flat; as the condition progresses the lesions enlarge and resemble vesicles that contain fluids. This is called a bullous lesion.
Recurrent Erythema Multiforme
If the lesions are treated, but re-emerges again after sometime, the condition is called recurrent erythema multiforme. This usually happens as result of HSV infection which was unresponsive to the previous treatment. Suppression of the virus and prophylactic treatment of acyclovir is employed to prevent recurrent erythema multiforme, but in some cases higher dosage of antivirals and dermatological treatments are needed to prevent recurring episodes.
Erythema Multiforme Pictures