High Grade Squamous Intraepithelial Lesion – Symptoms, Causes, Treatment
What is High Grade Squamous Intraepithelial Lesion (HGSIL)?
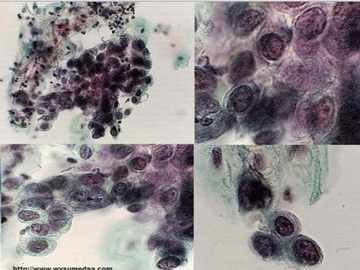
High grade squamous intraepithelial lesion or HSIL is a finding on the cervical tissues following a Pap smear. HSIL is a type of cervical dysplasia found in microscopic analysis of the cervical cells. Cervical dysplasia refers to the occurrence of pre-malignant or precancerous cells in the cervix and opening of the uterus. With this regard, HSIL indicates a moderate dysplasia to severe neoplasia of the cervical cells that may mean carcinoma in situ.
HSIL is different from low grade squamous intraepithelial lesion or LSIL in which the former have more defined changes in the shape and size of the cervical cells. LSIL only involve the appearance of early changes in the shape and size and is often associated with the presence of human papilloma virus or genital warts.
High grade squamous intraepithelial lesion may eventually lead to invasive cancer of the cervix when managements are not instituted. Being carcinoma in situ, it is considered stage 0 cervical cancer, but may not indicate that there is already cervical cancer. The presence of HSIL should be treated to prevent the development into cervical cancer.
High grade squamous intraepithelial neoplasia can be seen in various areas such as the esophagus, cervix, vagina and vulva, where there are squamous epitheliums.
Any detection of HSIL requires further tests to evaluate presence of cancer. Only 2% of patients with HSIL have invasive cancer, however up to 20% with HSIL will develop cancer if it is left untreated. Prevention of HSIL developing into cancer involves removing or destroying the precancerous cells.
Symptoms of HSIL
The appearance of cervical dysplasia such as the high grade squamous intraepithelial lesion usually does not result in signs and symptoms. The only manifestation of the condition is the microscopic changes that happen in the cervical cells evident upon microscopic examination. When HSIL occurs along with cervical cancer, there are symptoms associated with the cervical malignancy such as
- pain on the area
- bleeding after intercourse
- vaginal bleeding and
- abnormal vaginal secretions
Causes of HSIL
The cause of any type of cervical dysplasia such as the high grade squamous intraepithelial lesion is similar to the risk factors for cervical cancer, which includes:
Human Papilloma Virus
Infection with HPV or genital warts can lead to HSIL. This is spread through sexual contact and is one of the most common sexually transmitted diseases because of being asymptomatic sometimes. HPV usually affects young women aged 15 to 25 years old. Most women become infected with HPV without them knowing. HPV usually resolves spontaneously without any treatment, but it may have cause cervical dysplasia by that time if not treated. Recurrent HPV infection is commonly associated with cervical dysplasia and cervical cancer. Since HPV is transmitted through sexual contact, preventing it involves having only one sex partner and ensuring safe sex practices all the time. Increased risk for HPV infection involves having a reduced immune system or smoking.
Diagnosis of HSIL
Diagnostic Tests for high grade squamous intraepithelial lesion involves undergoing Pap smear. Pap smear or Pap test is done during pelvic examination where a speculum is inserted to collect samples of the cervical mucus. The mucus is then smeared and examined under the microscope. High grade squamous intraepithelial dysplasia of the cervix is then observed as the type of cervical dysplasia happening on the cervical cells.
When HSIL is observed, further tests are done to evaluate the presence of cervical cancer. These include:
Colposcopy
Colposcopy involves the use of a microscope or colposcope to study or visualize the cervix. Colposcopy helps identify specific areas of cervical dysplasia and can check the totality of the cervix. The abnormal cells may be removed at the time of colposcopy to prevent further spread. This management is called “see and treat”. Colposcopy may last for one hour and results are made depending on the extent of abnormality.
Biopsy
When suspicious areas are seen during colposcopy, a biopsy may be done to check if the cells are benign or malignant. Abnormal dysplasia in the cervix as seen in biopsies is termed cervical intraepithelial neoplasia (CIN). CIN is further classified into:
- CIN 1– This involves the presence of dysplasia on 1/3 portion of the cervical epithelium
- CIN 2– This involves the presence of dysplasia on the 2/3 portion of the cervical lining and is a more serious cervical dysplasia
- CIN 3– This can be categorized as carcinoma in situ in which the dysplasia affects more than 2/3 of the cervical lining.
HPV testing
HPV testing is also performed in women to detect presence of HPV infection.
Treatment of HSIL
The presence of cervical intraepithelial neoplasia in biopsy may prompt for treatments. Treatments include:
Loop Electrosurgical Excision Procedure or LEEP
This surgical procedure involves the excision of abnormal cells through the introduction of electric current through a wire loop in the cervix. When high grade squamous intraepithelial lesion is diagnosed in pregnant women, LEEP may be postponed and done after delivery because it can cause premature labor or spontaneous abortion in the first trimester. Progression of HSIL is usually slow during pregnancy so LEEP may be done later.
Conization
Conization is another approach in the treatment of HSIL. This involves the removal of a cone-shaped tissue from the cervix to get the deeper layers of abnormal cells and not just the superficial cervical lining. This is usually done during biopsy and is also called cone biopsy.
Cryotherapy
This surgical procedure involves the use of very cold substances to freeze the abnormal cervical cells. After freezing, the area exposed is usually removed.
Laser Therapy
This procedure involves the use of laser beams to destroy and remove the abnormal cells.
Follow Up Care
After the removal or the excision of the abnormal cervical cells, follow-up check-ups are needed to ascertain that no cervical cancer or another HSIL is taking place. Cells may still become abnormal, despite the surgical removal and may progress to cervical cancer when not detected early. Follow-up care includes:
- Pap smear with colposcopy every 6 months in one year followed by annual pap smears when there are no abnormal cells seen.
- Pap smear and colposcopy every 6 months when abnormal cells are seen after the first year of follow-up.
Prognosis of HSIL
The presence of HSIL should not be mistaken as presence of cancer. HSIL has a good prognosis when treatments are instituted. In fact, only 20% of cases progresses to cervical cancer without treatment, which means that early management for HSIL will not eventually lead to cervical malignancy.
Finally, Compare with – Low Grade Squamous Intraepithelial Lesion – Symptoms, Causes, Treatment