Mycosis Fungoides
Mycosis fungoides is the most common example of cutaneous T cell lymphoma. This condition may usually affect adults who are over 50 years of age but cases of children being affected have been reported [1, 2].
What is Mycosis Fungoides?
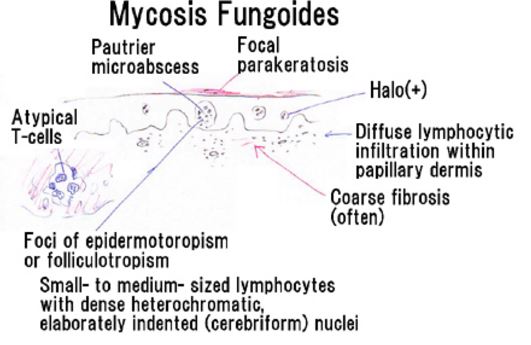
The disease condition of mycosis fungoides is an example of a blood cancer called as cutaneous T-cell lymphoma. In this malignancy, the T-cells of the blood become cancerous and affects the skin. The result is the appearance of different types of skin lesion. Although the lesions are on the skin, the skin cells do not become malignant [3, 4]. Figure 1 shows an example of lesions associated with mycosis fungoides.

Figure 1- Mycosis fungoides
The prognosis of this condition depends on several factors such as the age of the patient and the progression of the condition. Those who were diagnosed at the early phase of mycosis fungoides have a 5-year survival rate of 100% while those in the last phase of the condition have a 5-year survival rate of 14% [5].
Phases
The condition have a slow progression and undergoes several distinct stages. It is important to note that not everyone will undergo through all of the stages [1, 2, 6].
Premycotic phase
Most patients will develop flat and scaly lesions that are reddish or pinkish. The malignant T-cells are present in these lesions. These do not cause any symptoms and may last for several months or even years [1, 2, 6].
Patch phase
Eczema-like patches will appear in the body. They are commonly found in upper thighs, lower abdomen, breasts and buttocks [1, 2, 6].
Plaque phase
The plaques are reddish or brownish raised lesions. These plaques may develop from the patches or they may develop on their own. There are patients who have patches and plaques at the same time [1, 2, 6].
Tumor phase
Tumors that are deeper and thicker than plaques may develop. As before, the tumors may develop from existing patches and plaques or they can form on their own. There are times that these tumors will have open sores which increases the risk for infection. The cancerous T-cells may spread to other organs such as the lungs, liver, spleen and lymph nodes [1, 2, 6].
Causes
The exact cause of mycosis fungoides is still unknown but the DNA of the cancerous cells have shown chromosomal abnormalities. Examples of chromosomal changes include addition or loss of genetic material. Other causes that are being considered are viral or bacterial infections and environmental exposure [1, 4].
Risk Factors
Factors that may increase the likelihood of an individual to develop mycosis fungoides include advanced age, cigarette smoking, elevated body mass index, familial history of multiple myeloma and the presence eczema [7].
Signs and Symptoms
The primary symptoms of mycosis fungoides is the appearance of skin lesions. These lesions may be in the form of rash, patch, plaque or tumor in the skin. It is through the lesions that the stage of the disease is identified. Other symptoms that may be present include lymphadenopathy, hypercalcemia and enlarging of some organs or organomegaly [4].
Diagnosis
Health history and physical examination
As part of the health history, the physician will note the patient’s health habits and past illnesses. The physician will take note of the quantity and quality of the skin lesions during the physical examination. Photos may be even be taken to monitor the progression. Other symptoms that may be present will be identified as well [2, 4].
Skin biopsy
A sample of the patient’s skin will be collected by the physician and will be sent to a pathologist for an examination. This will be viewed under a microscope to check for the presence of cancer. Several skin biopsies may be performed before the diagnosis of mycosis fungoides is established [2, 4].
T-cell receptor gene arrangement test
The T-cells that are present in a tissue sample will be analysed. This test will identify any changes in the genes of the T-cell [2, 4].
Treatment
There are different types of treatment regimen that are used for the management of mycosis fungoides. The treatment depends on factors such as the lesions that are present and the progression of the condition [1, 2, 4].
Photodynamic therapy
This therapy involves a laser light and a drug that is injected to the vein of the patient. The drug collects more in cancer cells and is not active until it is exposed to the light. The result is the elimination of cancer cells while the normal cells of the body are barely harmed [1, 2, 4].
Chemotherapy
Chemotherapy uses antineoplastic drugs that may eliminate the cancer cells or prohibit them from growing. The combination of the drugs that will be used and the method of administration would depend on the stage of the condition [1, 2, 4].
Biologic therapy
This mode of therapy utilizes the patient’s immune system to eliminate the cancer cells. It may be strengthen with the use of substances that are either produced by the body or synthesized in a laboratory. This regimen is also known as biotherapy or immunotherapy [1, 2, 4].
Symptom relief
The skin lesions can be managed with the use of a corticosteroid or retinoids. A corticosteroid cream may relieve the swelling or inflammation of the skin while the use of retinoid is known to slow down the growth of certain cancer cells [1, 2, 4].
References
- US National Library of Medicine. (2016, May 25). Mycosis Fungoides. Retrieved from Genetics Home Reference: https://ghr.nlm.nih.gov/condition/mycosis-fungoides
- National Cancer Institute. (2016, February 5). Mycosis Fungoides and the Sézary Syndrome Treatment (PDQ®)–Patient Version. Retrieved from National Cancer Institute: http://www.cancer.gov/types/lymphoma/patient/mycosis-fungoides-treatment-pdq
- American Osteopathic College of Dermatology. (2015). Mycosis Fungoides. Retrieved from American Osteopathic College of Dermatology: http://www.aocd.org/page/MycosisFungoides
- Pinter-Brown, L. (2016, January 15). Cutaneous T-Cell Lymphoma. Retrieved from Medscape: http://emedicine.medscape.com/article/2139720-overview
- Stanford Medicine Multidisciplinary Cutaneous Lymphoma Group. (2016). Mycosis Fungoides/Sèzary Syndrome. Retrieved from Stanford Medicine Multidisciplinary Cutaneous Lymphoma Group: http://cutaneouslymphoma.stanford.edu/community/mycosis_fungoides.html
- Aschebrook-Kilroy, B., Cocco, P., & La Vecchia, C. (2014): The InterLymph Non-Hodgkin Lymphoma Subtypes Project. JNCI Monographs, 98-105.
- Kim, Y., & Liu, H. (2003). Long-term Outcome of 525 Patients With Mycosis Fungoides and Sézary Syndrome. JAMA Dermatology, 857-866.