Periorbital Cellulitis – Symptoms, Causes, Treatment & Home Remedies
What is Periorbital Cellulitis?
Periorbital cellulitis occurs when the eyelids and skin that surround the eyes are infected. This is due to infection made by pathogenic microorganisms that enter in the breaks of skin in the eye. It also doesn’t travel from an infected eye to the other. This medical condition affects children under the age of six. However, the inflammation can spread to the nasal sinuses causing sinusitis. A child’s risk for periorbital cellulitis can be increased when deep tooth and mouth infections are present, there is presence of styes or eyelid bumps and the lacrimal gland (the gland that produces tears) is swelling.
Periorbital cellulitis should not be confused with orbital cellulitis. Orbital cellulitis is a more serious problem and can be a life-threatening condition. The infection on orbital cellulitis is found on the septum of the orbit considering it as an ophthalmic emergency.
There are two different kinds of periorbital cellulitis. It depends on the soft tissue infected. These are:
- Preseptal cellulitis – this involves the eyelids and the tissues around the eye, but not affecting the eyeball. This type of infection can spread to different parts of the face but the orbital septum, the membrane that separates the orbit from the facial soft tissues, helps keep the orbit from being affected.
- Preseptal periorbital cellulitis – this is less serious since it doesn’t affect the eye and socket but it can spread to the orbit and it is always seen on small children.
Causes
There are different causes of periorbital cellulitis:
- Skin trauma or a break or laceration in the skin
- Infection brought about a bug or insect bite
- Spread of infection from paranasal sinuses or dacryocystitis
- Infection from the respiratory tract
Common causative agents in periorbital cellulitis are Staphylococcus epidermidis, Staphylococcus Aureus, Haemophilus Influenzae, Steptococcus and some anaerobic microorganisms.
Symptoms & Signs
Children can’t tell if they are having abnormalities in their body, therefore it is up to the parents to notice deviations from their children. Parents should see and observe marked changes on the face and in the eyes of the child. The symptoms manifested are:
- Tenderness around the affected area
- Swelling of eye lids
- Conjunctivitis or pink eye
- Low grade fever
- Only one eye is affected
- The child had difficulty in opening their affected eye lid
- There are red streaks on the skin of the eye
- The child becomes agitated
- The child has colds
- In some cases there would be presence of drainage coming from the eye
- The child’s eye movements and able to see are not affected
Immediate help is needed when:
- The child reports blurred or double vision
- The child reports photosensitivity
- The child experiences high fever and chills
- The child reports that his or her neck feels stiff and is unable to move it
- The child experiences seizure
Diagnosis
When the patient is brought to the hospital, an ophthalmologist will determine if the patient was suspected with cellulitis in the eye area. During this consultation, the patient’s medical history will be taken to determine the origin of the infection, recent sinus infection and dental problems. Physical exam will also be done to check deviations and abnormalities in the affected area. The following laboratory and diagnostic tests may also be needed to diagnose periorbital cellulitis
Blood Tests – This is done to determine what type and what kind of bacteria causes the infection.
Drainage culture – Same as with blood tests, this is done to determine the pathogen involved
Computed Tomography scan
Computed Tomography scan test will visualize your child’s eye structures such as bones, muscles and blood vessels around the eyes. A dye can be introduced to help in visualization. It is important to check first the child’s history of allergies to seafood and iodine to prevent anaphylactic reactions.
Treatment
Periorbital cellulitis treatment regimen includes:
- Giving of antibiotics for periorbital cellulitis.
For mild cases, oral antibiotics are prescribed to kill the pathogenic microorganism and prevent complications. Some of the antibiotics prescribed are: penicillin and co-amoxiclav in which it may be required to be taken seven to ten days for adults and for children affected, they may be asked to take it in three divided doses for twenty-four hours.
When cases are severe, the patient will be admitted to the hospital and IV antibiotics will be given two to three days. A drug which usually prescribed is Ceftriaxone 2mg of injection. Once the treatment is finished, the patient’s antibiotics will return into oral form to prevent the disease from recurring.
- Anti-inflammatory drugs are also given to reduce the child’s pain and inflammation such as ibuprofen.
- Medications for colds and eye drops or ointments are also prescribed.
- Tetanus vaccines are also given to prevent tetanus, a life-threatening infection because your child can acquire it from deep cuts and puncture wounds.
- Warm, moist compresses can also help soothe the affected area.
- For cases where there is lid abscess or sty, an eye specialist is needed to drain it.
To determine the effect of the treatment, the physician may require a follow-up visit, a week or a two later in which the infection should be long gone. This infection may clear up as little as 48 hours.
It is also important for the child to wear safety equipments to protect his or her face from injury. This is to guard the face from lacerations and trauma. In the event that a wound is present, it is advised to clean the affected area and keep it dry. The use of soap and water would be enough and covering the wounds with dry bandage will complete it. This is to prevent bacteria from harboring opened skin wounds.
Home Remedies
For adults, home remedies are suggested since they can determine which type is actually effective on them.
- The use of coriander seeds to use it to wash the eyes and face are essential to eye infection relief.
- Warm compresses of rose oil, lavender and chamomile help soothe the affected area.
- Oils with antibacterial properties such as tee tree oil can produce a faster recovery from the infection.
- Soaking of cloth into aloe vera juice will also help relax the infected eye.
Is Periorbital Cellulitis Contagious?
The periorbital cellulitis itself is not contagious, but the bacteria that cause periorbital cellulutis can cause other infection especially if it goes through the bloodstream.
Pictures
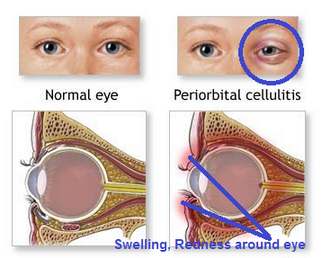
Picture of normal eye and periorbital cellulitis eye comparison

Picture of swelling, redness in children of periorbital cellulitis patients

Periorbital Cellulitis Image in women teenager (right eye)

Periorbital cellulitis diagnosis (look at the redness and odema of eye)

Purulent discharge from periorbital cellulitis eye

Severe form of periorbital cellulitis

CT scan (brain) showing periorbital cellulitis