Low Grade Squamous Intraepithelial Lesion – Symptoms, Causes, Treatment
What is Low Grade Squamous Intraepithelial Lesion (LSIL)?
One cell constitutes a single building block of the body. Everyone already knows that, even little children who have a basic grasp of human anatomy, but due to the current scourge of diseases like cancer, some of these cells that are supposed to build and protect the body have been transformed into ruthless attackers.
So now we have numerous conditions where a specific group of cells are trying to overtake the whole biological system, like acute lymphocytic leukemia for example. There is also a similar disease that is comparable to the former, though Low Grade Squamous Intraepithelial Lesion originates and mainly affects a different part of the body. So now, let us look at the importance of low grade squamous intraepithelial lesion and how it impacts the body of a human being, particularly in the case of women.
Let us start first with the “basics” before getting in to more detail. A squamous cell basically looks like a flat and plate like cell. Usually, this type of cell is more abundant at the edges of the epithelium. The epithelium is a part of the body which covers both the internal and external organs of the body separately.
More often, it also envelops the various parts of the body like the linings of the vessels, body cavities, glands, and organs of different systems and functions. The epithelium also consists of cells which are bound together by some connective material and varies in the number of layers and the kinds of cells.
There are also different types of squamous epithelial cells. There is the simple squamous epithelium, which only has one layer. Examples of this include mesothelium, endothelium, and pulmonary alveoli. The other, which is the stratified squamous epithelium, consists of a basal layer of cuboidal cells and other overlying layers of squamous cells. The epidermis that is a part of our skin, for example, comprises five different layers alone.
Having a low grade squamous intraepithelial lesion means that these otherwise normal cells have some abnormalities in them. The most commonly affected organ, at least for women, is the cervix. The verdict is still out with regards to what causes a low grade squamous intraepithelial lesion. The “culprit” is typically a minor injury that has healed in the cervix. The healing “process” has then caused these squamous cells to exhibit a rapid overgrowth that can only seem as unnatural for the affected patient.
Low Grade Squamous Intraepithelial Lesion Symptoms & Signs
Typically, a low grade squamous intraepithelial lesion will not manifest itself in its early incarnation. However, as the lesion spreads, the different signs and symptoms may appear.
Pruritus
Long-standing pruritus or itching and soreness are the most common initial manifestations of a low grade squamous intraepithelial lesion. Itching occurs in half of all the patients with these lesions.
Bleeding
Bleeding, foul-smelling discharge, and pain may also be present and are usually giveaway signs that the disease has indeed progressed. There may be some instances when the lesions may be visible and accessible and grow relatively slowly.
Early lesions may appear as chronic dermatitis or skin inflammation. Later on, some of these patients may also notice that a “lump” will then continue to grow and will eventually become a hard, ulcerated, and cauliflower-like in appearance.
Low Grade Squamous Intraepithelial Lesion Causes
As we have mentioned above, the exact cause of a low grade squamous intraepithelial lesion is still unknown. The only thing that most researchers can agree on is the possible risk factors of this condition.
Though a low grade squamous intraepithelial lesion in the cervix does not indicate that the patient is now experiencing cancer, it should serve as a “warning” sign that an occurrence of cancer may happen in the near future. Low grade squamous intraepithelial lesions represent 4% of all potential gynaecologic malignancies and are seen mostly in postmenopausal women. However, the incidence for younger women is also increasing. The median age for this condition is fifty years of age.
Other possible risk factors that women should be aware of with regards to a low grade squamous intraepithelial lesion are
- smoking,
- human papillomavirus (HPV) infection,
- human immunodeficiency virus (HIV) infection, and
- immunosuppression
The less common risk factors are
- bartholin’s gland cancer
- vulvar sarcoma and
- malignant melanoma.
LSIL Diagnosis & Treatment
As much as possible, gynaecologists everywhere are not recommending any kind of treatment to be done with a low grade squamous intraepithelial lesion. The reason is that, unless it has progressed to something far more severe, it should not be attempted to excise or remove the lesion in any way. The best thing that a patient can do is to just “wait”, however impatient patients may be for some drastic procedure to be done.
Gynaecologists or any health care professional is in an ideal position to encourage the patient to perform a vulvar self-examination test regularly using the aid of a mirror. With the mirror, the patient can see what constitutes a normal female anatomy and learn about any changes that should be reported, like the increase in size of the lesion, ulcers, masses, or even a persistent itching. The doctor should urge the patient to seek proper health care if anything abnormal is noticed to be happening inside. A regular pap test every four to six months should also be observed by the patient in question, as well.
However, there may be some cases when a gynaecologist may deem that the lesions may be progressing more rapidly than they had initially expected. In cases like these, some rather aggressive and diagnostic procedures can be employed by the attending physician. One of these is a colposcopy, an examination of the vagina and the cervix with an optical magnifying instrument, which is called a colposcope. A colposcopy is also commonly performed after a pap smear test in the treatment of cervical dysplasia, which is an abnormal tissue development of the uterine cervix. The most dangerous thing about having a cervical dysplasia is that, in about one out of ten cases which have been monitored over recent years, the atypical epithelium which the gynaecologist has observed earlier can progress to a full-blown carcinoma.
A biopsy may also be performed in lieu of a colposcopy. In this procedure, a small piece of living tissue from an organ or other part of the body is removed for microscopic examination.
The results from this examination can then confirm or establish a diagnosis. It can also estimate the prognosis of the client, or even follow the course of the disease. This kind of procedure is commonly used to determine whether the cancer is present or has spread inside the body.
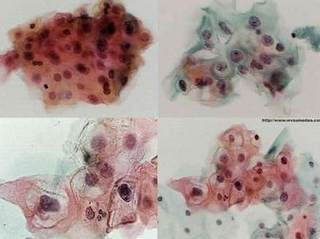
Picture 1 – Biopsy results of LSIL under electron microscope.
Prevention of LSIL
However, prevention may be as simple as decreasing the incidence of the risk factors associated with low grade squamous intraepithelial lesion. Some simple things, like abstaining from promiscuous sexual activity or having multiple sex partners, can be helpful in reducing the chances of this disease being aggravated.
Read & compare – High Grade Squamous Intraepithelial Lesion (HGSIL) – Symptoms, Causes, Treatment