What is Mucositis?
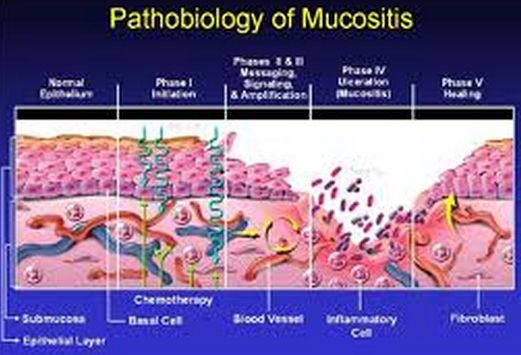
Clients undergoing chemotherapy for cancer frequently have mucositis (sores in mucous membranes) of the entire GI tract, especially in the mouth (stomatitis). Normally, the mucous membrane of the tract undergoes rapid cell division and replaces dead damaged cells quickly. In chemotherapy, mucous membrane cells are killed more rapidly than they are replaced resulting in sore formation. An individual may have a sensation a bit like getting burn in the throat. Mouth sores are painful and interfere with clients’ desire and ability to eat. The patients most likely may require medication for pain for a period of one week or two until the tissues get better.
Mucositis is the effect of modern cell-killing treatment for cancer patients. It is in addition the chief source of pain for patients who go through transplants for the bone marrow.
Symptoms & Signs
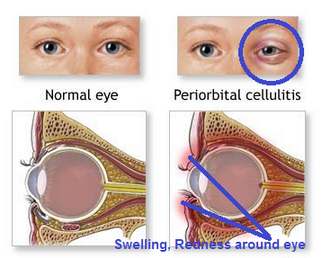
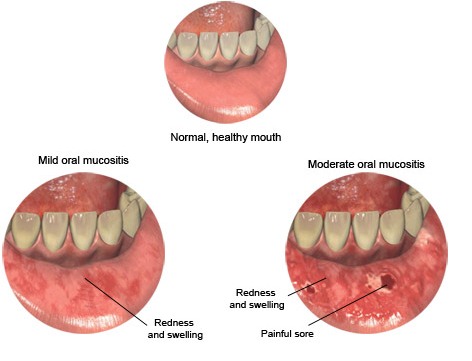
Mucositis because it is an inflammation of the mucous membranes it includes the symptoms of redness, pain and ulceration in the affected area.
Aside from the main symptoms, there are also numerous outcomes that may take place due to the occurrence of mucositis and these include.
- Decrease in the volume of blood (Hypovolemia)
- Fluid and electrolyte imbalances
- Malnutrition (underweight)
If the patient is not taken care of, these complications are possible to be deadly based on the extent of severity.
What makes it more complicated is that chemotherapy usually cause nausea and vomiting and what happens is that the mucous coating the inside of the mouth are predominantly susceptible and at risk to contamination and ulceration. Furthermore, vomiting can cause the mouth’s lining and the gastrointestinal tract to become aggravated. The damaged cells in the mucosal lining will be incapable of healing normally.
An additional effect of this condition is the loss of taste. This adds to the amount of the power and assertiveness of the chemotherapy that the patient is having. Due to the mouth sores, eating will be very difficult and will be even harder if you are unable to taste the food you are eating. If you cannot eat properly you will start to have weight loss and eventually will also lose the integrity of the muscles. They will have deficiency in energy and therefore will have a weakened immunity.
Causes & Risk Factors
1. Chemotherapy
- Can get in the way of eating, drinking, and living
- Can be a reason for an increased risk of infection, reduction of appetite, and interruption in cancer management
- Will make the person with mucositis miserable
Sores can appear five to ten days after chemotherapy starts and their level of severity and occurrence will be based on the particular chemotherapy
Frequently, patients require high doses of chemotherapeutic agents, or combined chemotherapy and radiation for stem cell or bone marrow transplants preparation. Unfortunately, such high doses clean out the bone marrow and this amplify the probability of mouth sores
Chemotrapeutic drugs such as Doxorubicin, or vincristine, 5-FU and methotrexate, or taxoids like docetaxel frequently cause mucositis
2. Radiation
Radiation in the head or neck area can cause mucositis
Both of them show aggression in cells for the period of their separation process. Therefore, cells that separate quickly, like those in the lining of the mouth which separates every three days are frequently involve. This can produce mouth sores since the cells that are assaulted die and do not rejuvenate. When they don’t rejuvenate, the result will be mouth ulcers. Also, a reduced white blood count can make the sores emerge more commonly and also strengthen the risk of infection.
Grading
World Health Organization’s Oral Toxicity Scale
Grade 1 – Pain and redness
Grade 2 – Redness, ulcers, swallowing solid food is possible
Grade 3 – Ulcers with widespread redness; swallowing solid food is not possible
Grade 4 – Mucositis to the degree that receiving nourishment is not possible
Treatment
Infection control
In treating mucositis experts agree that to lessen the infection brought about by mouth sores keeping good mouth hygiene is still the best way.
The cleaning of the mouth is very important. Infections make the lives of patients undergoing chemotherapy and radiation difficult. Given that the mouth in nature shelters microorganisms like bacteria and fungi, it’s vital to maintain the mouth’s hygiene in an attempt to avoid contaminations.
The regularity of treatment is the most principal aspect in decreasing the gravity of disease and in upholding the healing of the ulcers. It is advisable to clean the teeth and mouth every four hours or after each meal and before going to sleep.
It is recommended to brush the teeth softly and to pay careful attention on your gum line. Brush two to three times daily using soft, bristled brush made up of nylon. If they don’t cause distress to the mouth, electric and ultrasonic brushes may be used. Foam brush or piece of gauze is more preferred by some health professionals who say that it’s safer to not use a brush to clean the mouth. The gauze can be washed in water with salt or prescribed mouthwash. In cases wherein there’s a low platelet count (fewer than 20,000) or low absolute neutrophil count (fewer than 500) it is necessary to use either the foam brush or gauze instead.
When a pediatric client used floss it is recommended to use waxed or taped floss to aid in the prevention of further damage to soft tissue, but it is absolutely necessary for the child to not floss if his ANC is 500 or less.
Secondary infection control
To avoid secondary infection the doctor may prescribe antivirals and antibacterials such as Nystatin, Acyclovir, Clotrimazole, Fluconazole, etc.
Mucositis caused by Radiation or chemotherapy
At present there is no recognized way of avoiding mouth sores caused by chemotherapy or radiation.
Pictures
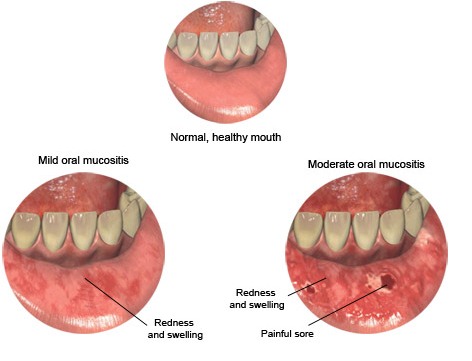
Mucositis picture – redness, swelling, sore of mucus membrane of lips
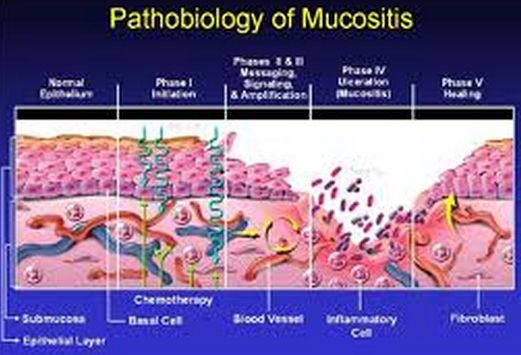
Image of Pathobiology of mucositis

Image of Mucositis of lips in teenagers

Mucositis picture showing redness, swelling, ulcer of mucus membrane

Picture of grade 2 mucositis

Picture of Grade 4 mucositis