Prolapsed Bladder – Symptoms, Causes, Treatment and Pictures
What is Prolapsed Bladder?
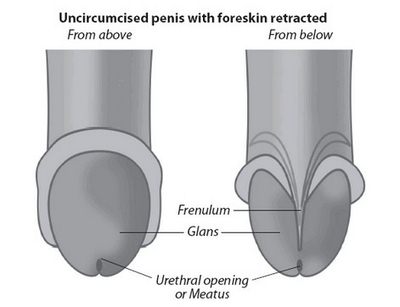
Bladder is a balloon shaped, hollow muscular organ that collects urine from the kidney and store it before it goes out of the body through urination. Bladder distends when it is full and return on its normal size when emptied. In males, the base of the bladder is located between the rectum and symphysis pubic, and above the prostate gland. In females, the bladder lies inferior to uterus and ahead to the vagina. The size of the bladder is about the shape of a pear when empty, its normal capacity is 400ml to 600ml.
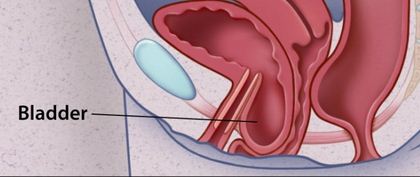
Prolapsed Bladder or also called Cystocele is a condition when the muscle between women’s bladder and vagina fall out of place, and sticks out into vagina.
It is more common among women with Hispanic and Asian of descents, however African-American women have a reduced risk of having Prolapsed bladder.
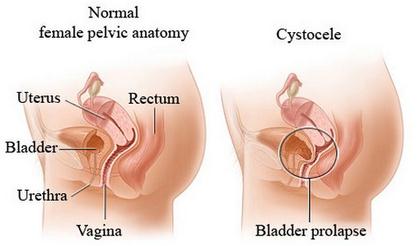
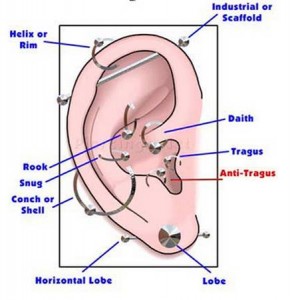
Picture – Prolapsed bladder (cystocele)
Source – revolutionhealth.com
Prolapsed Bladder Pathophysiology
Organs of the Pelvic is primarily supported by connective tissue called Levator Ani Muscle and Endoplevic tissue. It connects the organs to the pelvic muscle and bones. Bladder prolapses when this support muscle gets weak due to different causes like trauma and injury.
The listed below are the confirmed risk factors of Prolapsed Bladder:
- Age
- Vaginal Delivery
- Increasing parity
- Overwight and Obesity
- Congenital disorder like Spina Bifida and Spina Bifida occulta
Prolapsed bladder is divided in 4 stages, depending on the degree of displacement.
- Grade one (Mild) – Small part of the bladder droop in the vagina
- Grade two (Moderate) – The bladder falls enough and able to reach the opening of the vagina.
- Grade Three (Severe) – The bladder extends up to the vagina’s opening.
- Grade Four (Complete) – The bladder falls out completely outside the opening of the vagina.
Signs and Symptoms
Patients may not notice symptoms during the first few days or weeks, but after some time as the condition develops symptoms can be felt and became noticeable.
They may include:
- Piece of tissue is felt in the vagina – Tissue is felt in the vaginal opening because the bladder droops in the vagina. It is more obvious while sitting but disppear while you lie down.
- Dysuria or Difficulty urinating – As the bladder drops in the vagina, the urine cannot flow freely enough to come out to the urethra.
- Incontinence – Leakage of urine when you sneeze, cough and laugh. In worst cases, patient totally cannot control urination.
- Pain in the Pelvic Area – The pain is commonly felt in the Lower back.
- Incomplete voiding – Feeling that bladder is not emptied after urinating.
- Urinary tract infection – Infection that happens repetitive. Since the bladder drops, the urine cannot freely come out from bladder to flow in the ureters. The result will be the urine will remain in the bladder causing presence of microorganism that will cause infection.
- Painful sexual intercourse or dyspareunia – The bladder covers the space in the vaginal opening causing pain and discomfort during sexual activity.
Causes of Prolapsed Bladder
Pelvic muscles are connective tissue that support your bladder, uterus and rectum, these organs composed the pelvic cavity. When these muscle start to looses its strength and became weaker there will be a large possibility of having bladder prolapse.
These are the following cause of developing bladder prolapse:
- Pregnancy – Pregnancy is one most common causes, especially in woman who have multiple pregnancies. As the fetus inside the womb grow it gets bigger and heavier making more pressure on the pelvic muscle. Some muscles cannot carry enough the weight resulting to stretching and losing muscle strength.
- Giving Birth – During labor and delivery, the pelvic muscle and ligament that support the vagina experience overexertion resulting to muscle strain. The muscle cannot support enough the muscle and eventually the bladder will loose it position.
- Menopause – Estrogen is a hormone produced by the body and one of its function is to keep the vaginal muscle strong. During menopausal period, the body stops from producing estrogen, making the vaginal muscle weaker.
- Strenuous activity – Lifting heavy objects, straining during bowel movement, forceful cough may cause straining in the pelvic muscle.
- Overweight and Obesity – Being heavy weight is also one of the top risks in developing prolapse bladder.
Diagnosis
- Pelvic and Perineal examination – The doctor will inspect for presence of protruded muscle within the vagina. The doctor will also assess the muscle strength by asking you to contract the pelvic muscle.
- Voiding Cystourethrogram – Examination of the bladder and urethra done while the bladder fills and empties. Using a radiopaque liquid placed by means of a catheter, radio-graphs are taken before, during and after voiding. This test can determine any deformities and irregularities in the appearance and function of the bladder.
- Cystoscopy – Is a non-invasive procedure done to see the inside view of the urinary tract. Using a scope, the doctor can determine if there are any abnormalities in the bladder, ureter and urethra.
Treatment
Treatment for prolapse bladder depends on the condition
Grade 1 – For mild cases and situation with no obvious symptoms may require no treament. Kegels Exercise is one of recommended activity because it helps strengthen pelvic muscle. Stay away from Lifting heavy object and straining to avoid worsening the condition.
If the situation gets worse, your Doctor may recommend non surgical treatment. This includes:
1. Pessary
It is a device place in the vagina to support the bladder to maintain its position. Removal and regular cleaning of Pessaries must be observed to prevent infection.
2. Estrogen Therapy
Estrogen is a hormone that strengthen the vaginal muscle. Since it is only present when women still have Menstrual period, Menopause women are at risk of having Prolapse bladder. This estrogen replacement can supply women of the loss hormone to prevent weakened vaginal muscle that may eventually lead to Prolapsed bladder.
In some cases, symptoms continue and became more serious. Surgery can be an option at this time to relieve symptoms that are connected to Prolapsed Bladder.
This may include:
3. Vaginal Repair (surgery)
It is done by a surgeon to lift the bladder on its original normal position. It also includes taking off unnecessary tissues and tightening layers of pelvic muscle and ligaments.
4. Hysterectomy
If the condition recurs another surgery is needed. If prolapsed uterus occurs the doctor may recommend removal of uterus or Hysterectomy. This procedure may help in relieving symptoms, but it prevents you to bear child.
Complications of Prolapsed Bladder
Complications secondary to Bladder prolapse is not common, but it is benificial to know what are the possible condition that may arise due to Prolapsed Bladder.
- Pain – Bladder prolapsed can cause vaginal, groin, lower pelvic and abdominal pain.
- Bowel, bladder and sexual dysfunctions – If left untreated, bladder prolapsed may interfere in your bowel movement, bladder and sexual functions.