Papilledema – Definition, Pictures, Causes, Symptoms, Treatment
Papilledema Definition
Papilledema is the swelling of the optic disc caused by increased intracranial pressure. The swelling in the optic disc causes problems on the vision and may cause permanent vision loss when not managed. However, acute papilledema may result to preservation of vision.
The occurrence of papilledema usually develops over hours to weeks of increased intracranial pressure. The term Papilledema is only used correctly when it describes optic disc swelling as a result of increased intracranial pressure. Optic disc swelling with the presence of underlying infection and inflammation of the optic nerve is different from papilledema.
The optic nerve is anatomically continuous with the brain through the subarachnoid space. Any increase in pressure in the cranium thereby is being transmitted to the optic nerve. The anterior end of the optic nerve discontinues at the eye, thereby causing protrusion of the optic nerve on the area.
This results in the bulging of the ganglion cells of the optic disc. The prolonged and unmanaged edema of the optic nerve causes loss of the fibers of the ganglion cells and subsequently, impairment in the vision.
The incidence of papilledema is equal in men and women and may also occur at any age as long as the causes are present.
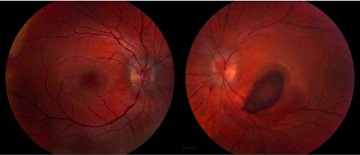
Optic disk edema
Image source: webeye.ophth.uiowa.edu
Types of Papilledema
Bilateral Papilledema
Papilledema most commonly occur as bilateral, which means that both eyes are affected. Since the optic nerve is connected with the subarachnoid space, both sides of the optic nerve receive transmission of an increased intracranial pressure. The presence of bilateral papilledema usually rules out possible problems specific to the eyes that may cause swelling.
Unilateral Papilledema
Unilateral papilledema is a rare occurrence. Unilateral papilledema has only been documented few times. The development of disc swelling in only one eye implicates the occurrence of other etiologic phenomenon.
Grading of Papilledema
- Stage 0 – This stage describes normal pressure in the optic disc.
- Stage 1 – This involves very early papilledema where there is obscuration of the disc in the nasal border.
- Stage 2 – This stage involves the presence of obscurations of all borders with elevation of nasal border. This is described as early papilledema.
- Stage 3 – There is already increased optic nerve head diameter and considered moderate papilledema.
- Stage 4 – This is marked papilledema involving total elevation of the nerve head with peripapillary halo and total obscurations.
- Stage 5 – Severe papilledema involves obliteration of the optic cup and anterior expansion of the head of the optic nerve representing severe damage on the nerve.
Papilledema Symptoms
Papilledema is usually asymptomatic during the early stage of the condition. When symptoms occur, they include:
Headache
Headache occurs as a result of the increased intracranial pressure. Headache is usually an early sign of increased intracranial pressure and a developing papilledema. The nerves become compressed as a result of high pressure leading to severe headache. Headache usually becomes severe upon awakening and become worsened by Valsalva maneuver such as coughing and straining on stools.
Nausea and Vomiting
The increased intracranial pressure also puts pressure in the vomiting center of the brain, which is the medulla oblongata. The characteristic vomiting of increased ICP is projectile vomiting.
Blurring of Vision
The swelling of the optic disc causes the disturbance in the vision because the nerves are responsible for the sensory function of the eyes.
Visual Obscurations
This involves inability to see in certain areas of the visual field as a result of optic disc swelling also termed as blind spots.
Loss of vision
When the swelling becomes persistent, the optic nerve becomes permanently damaged leading to visual loss. The occurrence of visual loss happens during the last stage of the condition.
The eyes are examined using an opthalmoscope and may reveal loss of venous pulsation, venous engorgement, hemorrhages, optic disc elevation and radial retinal lines termed as Paton’s lines.
Papilledema Causes
Causes of papilledema include all factors that may increase the intracranial pressure such as:
- Space occupying lesions or tumors in the CNS – The cranium and the vertebrae is a closed system, which means that any foreign body or tumor in the area causes the pressure to increase leading to increased intracranial pressure.
- Decreased CSF resorption – The CSF is continuously circulated in the ventricles in the CNS. The CSF is also reabsorbed to make way for new CSF to be circulated. However, in the cases of inflammation in the meninges or venous sinus thrombosis, the CSF is poorly reabsorbed thereby increasing the circulating CSF and pressure inside the cranium.
- Idiopathic Intracranial Hypertension – This is an increase in the pressure in the arteries inside the cranium leading to increased pressure inside the cranium.
- Cerebral edema – Cerebral edema is a result of various medical conditions. It is commonly caused by trauma in infection. The edema or swelling increases the pressure and thereby leading to papilledema.
- Medications – Medications such as corticosteroids, minocycline, Accutane, lithium and nalidixic acid causes increased intracranial pressure during drug withdrawal and overdose.
Papilledema Diagnosis
The diagnosis of papilledema relies on the use of slit lamp examination and opthalmoscopy showing a characteristic of the optic nerve disc. The diagnostic tests are done when new onset headache is noted with possible increased intracranial pressure. Aside from the optic nerve diagnosis, a biopsy can be made to detect whether the tumor is benign or malignant whenever it is present.
Papilledema Image
Differential Diagnosis
Papilledema is usually differentiated from other conditions involving the eyes such as papillitis, optic neuritis, glaucoma, and retinal detachment.
Papilledema Treatment
The treatment of papilledema is primarily focused on the treatment of the underlying cause of the increased intracranial pressure. The direct cause, which is increased intracranial pressure, can be managed using the following treatments:
Diuretic Administration
The use of diuretics such as lasix and acetazolamide increases the adsorption of CSF to be eliminated through the urine.
Steroids
Steroids are potent anti-inflammatory medications and may be given for patients with cerebral edema. However, steroid use should be monitored because any abrupt change in the dosage may also cause increased ICP.
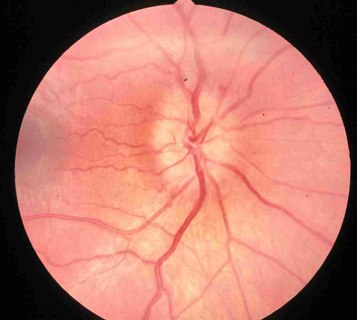
Surgical Approach
Repeated lumbar punctures are usually done to remove excess CSF in the spine thereby reducing the overall circulating CSF in the brain.

Lumbar puncture to remove excess CSF
Medication Modifciation
Medications causing the increased ICP should be stopped to prevent further increase in pressure.
Papillitis Vs. Papilledema
Papillitis is a condition of optic neuritis. It is called intraocular optic neuritis wherein there is inflammation of the optic nerve head. Papilledema on the other hand, is the bulging or swelling of the optic disc. Papillitis involves significant loss in the visual field and pain on the globe of the eyes, which is not present in papilledema.